Juvenile idiopathic arthritis, also called JIA, is a chronic inflammatory disease in childhood and often persists through adulthood and can result in severe disability. Biological treatments are an important therapeutic option for treating patients with JIA. This article will discuss the case study of severe and refractory polyarticular JIA with positive rheumatoid factor affecting children successfully treated with rituximab. You will also get to know about July Juvenile arthritis awareness Month.
While there’s a common misconception that only older individuals deal with arthritis, about 300,000 children in the US have been diagnosed with JIA. During National Juvenile Arthritis Awareness Month, it is important to note that children with JIA suffer from autoimmune and inflammatory conditions that can develop in children ages 16 and younger.
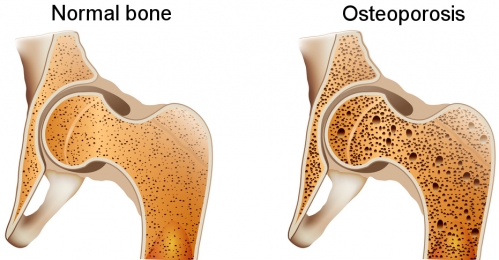
JIA is the most common rheumatological disease that affects children. It is characterized by arthritis with onset before age 16, lasting more than six weeks, and no other cause identified. Children with arthritis often present with swelling, joint pain, and morning stiffness. Juvenile arthritis symptoms may also be subtle, including limp and unusual posturing. The most serious complication of JIA is ocular inflammation that is often symptomatic but may be sight-threatening. A child’s immune system is not fully developed until age 18, so an autoimmune type of arthritis is especially a serious issue in children, compromising their ability to fight normal diseases and increasing the risk for complications that affect bone growth, their eyes, and more. Considered the most common form of arthritis, JIA is subcategorized as polyarthritis, systemic, enthesitis-related, oligoarthritis, or juvenile psoriatic arthritis.
The most important step in treating JIA is getting an accurate diagnosis, which can be long. While there is no cure for chronic childhood arthritis, remission is possible with early diagnosis and aggressive treatment. The treatment aims to relieve inflammation, treat pain and improve one’s quality of life.
About prevalence of JIA & genetic connection
Across the world, approximately a million children and young adults are dealing with juvenile arthritis, and the prevalence rate is consistently higher in girls. Africa and Middle Eastern countries add up to a diverse group of socioeconomic conditions, ethnicities, and climates that affect the prevalence of JIA. However, there is too little evidence from the region. Oligoarticular arthritis is more prevalent in such regions. Higher prevalence may be due to a huge unmet need in the region for local treatment guidelines, disease awareness, and timely diagnosis. Not enough pediatric rheumatologists also contribute to the challenges associated with managing JIA in these countries.
Most cases of JIA occur in people with no family history of the disorder. A small percentage of cases of JIA have been reported to be hereditary; however, the condition’s hereditary pattern is still unclear. A sibling of affected children is more likely to develop than the general population.
The case studies can help us understand JIA and its treatment
A 17-year-old African female with a five-year history of refractory polyarticular JIA (more than four affected joints during the first six months of illness) with positive rheumatoid factor as active JIA disease. During these five years, her disease involved multiple joints, such as the shoulders, wrists, ankles, hips, and finger joints, leading to deformities on her fingers. Reports of her physical examination show severe growth retardation. Deterioration of functional joints occurred, and she could no longer stand or walk. Also, experiencing severe hip pain and numerous joint deformities.
The patient first received methotrexate and corticosteroids, which showed no improvement. After that, rituximab was used weekly for a month along with concomitant methotrexate 10 mg weekly and bisphosphonate with a high dose of Vitamin D and calcium. Improvement has been seen within several weeks, and there is also a significant reduction in the intensity of her joint pain.
She was an 18-year-old African female presented with an 8-year history of refractory polyarticular JIA, again with a positive refractory factor. Her physical examination found a deformity of the left fourth finger, reduced range of motion of the left wrist, and reduced flexion of the knees. The patient was treated with methotrexate as well as with methotrexate and steroids for six years with improvement. Because of the activity and severity of the disease, treatment with rituximab was started in two infusions 15 days apart, with good clinical apart. The patient is undergoing sustained remission lasting six months, with no evidence of systemic inflammation.
Discussion
Generally, treatment aims to eliminate active disease, normalize joint function, preserve normal growth, and prevent patient disability and long-term joint damage. Until now, methotrexate has been one of the most common drugs for treating patients with JIA, with effectiveness and safety that satisfy the current criteria of evidence-based drug. However, conventional immunosuppressants show no improvement in almost 50% of patients as they cannot adequately control JIA symptoms or prevent further joint destruction, and they frequently cause side effects that limit their use. Biologic agents are classified as genetically engineered medicines designed to block the cytokines’ effects in JIA. Because of its effectiveness, there has been a rapid increase in the number and types of agents available to treat JIA. Much of the treatment of childhood arthritis decided on experience gained from adult patients and research studies.
Rituximab is a well-known medicinal treatment option in adult rheumatoid arthritis. However, it has not been regularly studied in JIA so far. But it has successfully induced the remission of childhood arthritis and reduced extra-articular manifestations without the need for oral prednisolone administration. This suggests that rituximab might be a promising therapeutic option in severe refractory JIA. Research reports fully support the results of the rituximab effectiveness and safety study. Rituximab was clinically approved for the treatment of rheumatoid arthritis in adults. Still, its usefulness in treating childhood arthritis or juvenile ankylosing spondylitis (arthritis that mostly affects the spines and the location where tendons, muscles and ligaments are stuck to bones) deserves to be proven. Further investigation is recommended.
Raising Awareness
July is National Juvenile arthritis awareness month. If your child or your loved one is dealing with JIA, connect to an organization that helps you learn how to conquer this illness from an early age and how to remain active for a lifetime. You can learn more about JIA by visiting the organization’s programs dedicated to rheumatoid arthritis. Also, sharing success stories and inspirational journeys helps raise awareness about the condition.
The bottom line
According to the research report of the above case study, the use of rituximab in the treatment of JIA, especially the subtype- polyarticular with positive rheumatoid factor, might be a good alternative. Larger clinical needs to be conducted in this direction to improve the effectiveness of the biotherapy for JIA. This July, find life-changing resources for your child or your loved one dealing with JIA and meet other families and experts who understand the condition well.